THE EU MEDICAL DEVICES REGULATION AND THE CORE-MD PROJECT
The European Union (EU) has a competitive and innovative medical devices sector with over 500 000 types of medical devices and in vitro medical devices placed on its market. The EU Medical Devices Regulation (MDR – Regulation (EU) 2017/745) lays down the rules regarding the placing on the market, making available on the market or putting into service of medical devices for human use (and accessories for such devices). The Regulation (EU) 2017/746 sets out the rules on in vitro diagnostic medical devices (IVDR).
The MDR has entered in force on May 26th this year and, among other points, there was an increase in the requirements for clinical evidence on high-risk medical devices. This has raised some concerns among the manufacturers of medical devices, particularly regarding possible market access delays and innovation. In Europe, there are more than 50% implantable medical devices classified as high-risk (e.g., heart valves, hip replacements, etc.) used in cardiology and orthopedics.
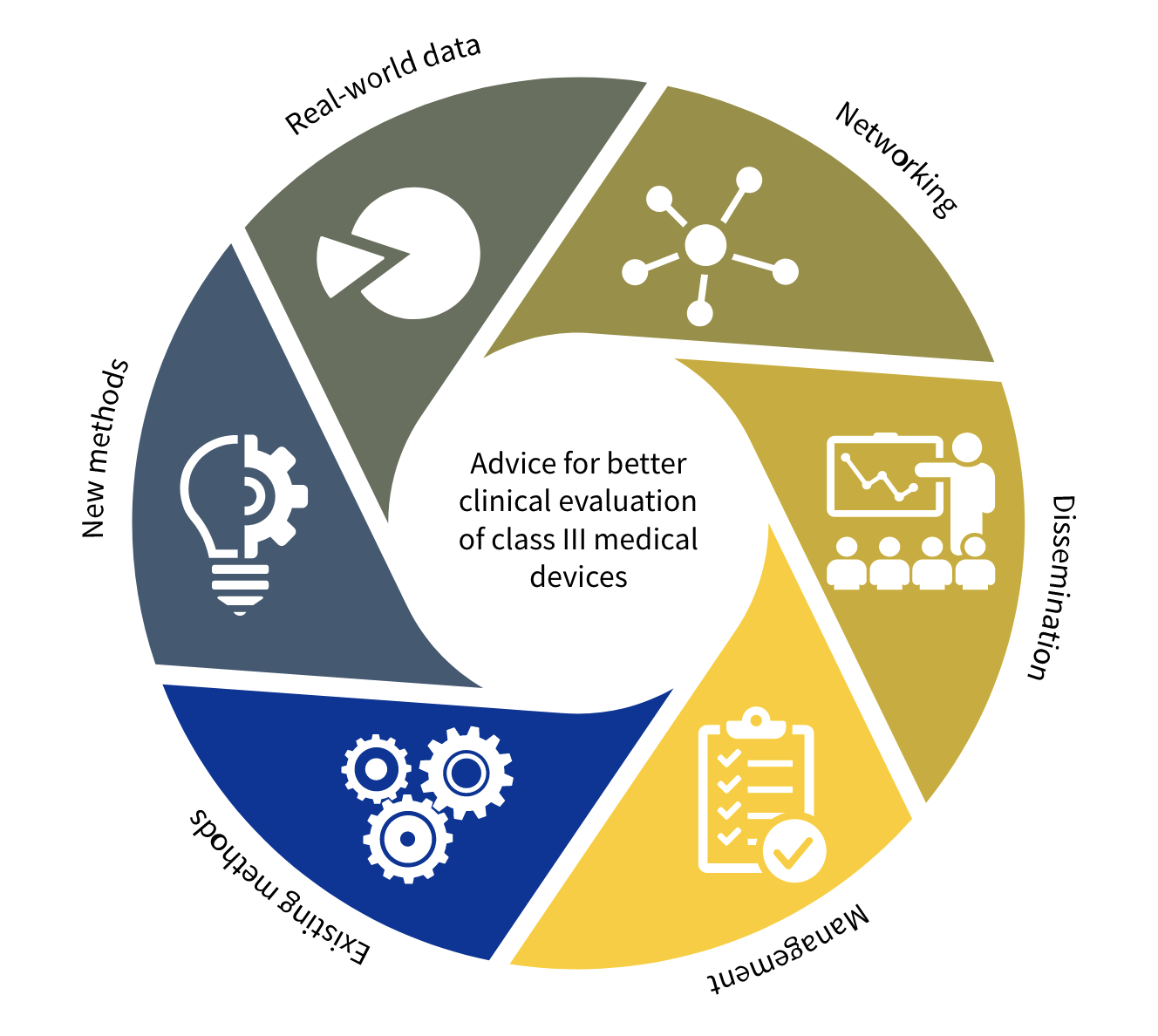
The Coordinating Research and Evidence for Medical Devices (CORE-MD) is an European Union Horizon 2020 project. The mission of CORE-MD is “translating expert knowledge into advice for EU regulatory guidance, and building expertise in regulatory science in the clinical community”. CORE-MD will translate expert scientific and clinical evidence on study designs for evaluating high-risk medical devices into advice for EU regulators, to achieve an appropriate balance between innovation, safety, and effectiveness.
Cardiology and Orthopedics will be areas of focus of the CORE-MD. The project started in April 2021 and will run until March 2024. It is led by the European Society of Cardiology (ESC), in close partnership with the European Federation of National Associations of Orthopedics and Traumatology (EFFORT). The CORE-MD consortium gets together medical associations, EU regulators, national public health institutes, notified bodies, academic institutions, patient’s groups and health technology assessment agencies. Manufacturer’s trade associations also participate. This project involves 35 specialist medical associations, which are members of the Biomedical Alliance in Europe.
The CORE-MD project is composed by five Work Packages.
Work Package 1 will review and summarise the designs of studies that have generated clinical evidence about the performance high-risk medical devices. Specifically, it will collect evidence concerning high-risk (class III) permanently implanted devices in the fields of cardiology and orthopaedics, as well as high-risk devices used for the treatment of diabetes mellitus. Its objectives are:
- To perform a systematic review of recommendations for the performance of clinical investigations and trials of high-risk medical devices, identifying their concordance and discordance.
- To perform a systematic review of the methodologies of clinical investigations that have been used to evaluate high-risk cardiovascular, orthopaedic and diabetic medical devices, identifying problems and ranking study designs for their quality and appropriateness.
- To review appropriate statistical methods for evaluating studies of high-risk medical devices.
- To review the utility of patient-reported outcome measures and patient-reported experience measures to generate premarket and post-market clinical evidence for high-risk devices, including independent review of their validity and accuracy
Work Package 2 will evaluate how evidence should be generated for innovative medical devices during first-in-human studies and early clinical trials. New methods of generating evidence will be considered and methods for evaluating high-risk devices for children will be assessed. Guidance for the evaluation of artificial intelligence in medical devices and standalone software as a medical device will be reviewed and developed. Its objectives are:
- To review and recommend alternative designs of clinical studies that can be used to provide high-quality clinical evidence for new high-risk medical devices.
- To conduct feasibility studies of using the IDEAL framework in the early stages of device clinical testing.
- To survey existing guidance and recommend criteria for the clinical evaluation and regulatory conformity assessment of artificial intelligence and machine learning in high-risk medical devices.
- To review and recommend methods for evaluating high-risk medical devices used in children.
Work Package 3 will explore methods to obtain and combine best clinical and scientific real-world evidence on clinical performance of high-risk medical devices in daily practice (post-marketing phase, for example from registries). It will also investigate how Notified Bodies are applying conditions to certificates of conformity. Its objectives are:
- To review and develop methods for aggregating clinical data from real-world sources and registries across the lifecycle of high-risk medical devices.
- To develop a web-based tool for the automated surveillance of reports relating to specific types of medical devices.
- To advise how post-market clinical evidence should be generated, based on an analysis of notified bodies’ practices in applying conditions to certificates of conformity.
Work Package 4 will provide the forum for all stakeholders to exchange best practices and collectively review the evidence generated, adopt position papers and recommendations. Its objectives are:
- To develop a charter for ethical practice related to clinical investigations of innovative high-risk medical devices.
- To approve CORE–MD proposals for a hierarchy of levels of clinical evidence for high-risk medical devices.
- To recommend how EU regulatory systems can implement new methodologies for clinical investigations of high-risk medical devices, using evidence generated across their whole life cycle.
- To identify the training needs of all stakeholders to enhance their expertise in methodologies for the assessment of high-risk medical devices, and develop appropriate educational objectives.
- To disseminate the publications, educational resources, and outcomes of CORE-MD as widely as possible to the clinical community and all stakeholders through newsletters, webinars, and social media.
Work Package 5 will coordinate and administer the project in technical and administrative terms.
If you wish to get more information about the EU Medical Devices Regulation (MDR – Regulation (EU) 2017/745), do not hesitate to contact us at info@criticalcatalyst.com.
References:
- Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on medical devices. Available at: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:02017R0745-20200424&from=EN
- Regulation (EU) 2017/746 of the European Parliament and of the Council of 5 April 2017 on in vitro diagnostic medical devices. Available at: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:02017R0746-20170505&from=EN
- CORE-MD. Coordinating Research and Evidence for Medical Devices. About the initiative. Available from: https://www.core-md.eu/about-the-initiative/